Leave Your Message
Biological Membrane Infection mechanisms play a crucial role in how pathogens invade host cells, leading to diverse diseases that challenge global health systems. According to the World Health Organization, infections caused by membrane-dwelling pathogens account for nearly 15% of all deaths worldwide, signifying an urgent need for deeper understanding and innovative approaches to combat these infections. Recent advancements in molecular biology and immunology have revealed intricate processes, such as how pathogens exploit the host's biological membranes to facilitate entry and establish infection. This blog aims to delve into the complexity of Biological Membrane Infection, exploring various types of mechanisms, their implications for health, and potential therapeutic targets that may pave the way for novel interventions in infectious disease management. Understanding these sophisticated interactions is essential for developing effective strategies to prevent and treat membrane-related infections efficiently.
Biological membranes serve as critical barriers between pathogens and host cells, playing a pivotal role in the entry and survival of infectious agents. The lipid bilayer structure of these membranes provides a selective permeability that pathogens exploit to infiltrate host systems. Understanding how pathogens interact with these membranes can illuminate potential prevention strategies. For instance, many viruses and bacteria use specific receptors on the host's membrane to gain entry, a process that varies widely among different pathogens.
Tip: To enhance your immunity against infections, consider maintaining a healthy diet rich in antioxidants and vital nutrients. These can bolster the body’s cell membranes, making it harder for pathogens to attach and invade.
Moreover, once inside, pathogens can manipulate membrane dynamics to evade the host's immune response. They can create modifications on the membrane surface that camouflage them or induce host cells to engulf them without triggering an alarm. This ineffectiveness of the immune response highlights the need for innovative therapeutic approaches aimed at disrupting these interactions.
Tip: Regular physical activity can boost your immune system, enhancing the integrity of cellular membranes and improving your body's overall defense mechanisms against infections.
 Biological membranes serve as the first line of defense against viral infections, acting as selective barriers that protect cells from harmful entities. However, viruses have evolved intricate mechanisms to disrupt these membranes, facilitating their entry into host cells. One major pathway involves the direct fusion of viral envelopes with cellular membranes, often mediated by specific viral proteins that alter membrane fluidity, creating openings for viral genomes to enter. Additionally, some viruses exploit endocytic pathways, hijacking the cell's own machinery to gain access beneath the membrane surface.
Biological membranes serve as the first line of defense against viral infections, acting as selective barriers that protect cells from harmful entities. However, viruses have evolved intricate mechanisms to disrupt these membranes, facilitating their entry into host cells. One major pathway involves the direct fusion of viral envelopes with cellular membranes, often mediated by specific viral proteins that alter membrane fluidity, creating openings for viral genomes to enter. Additionally, some viruses exploit endocytic pathways, hijacking the cell's own machinery to gain access beneath the membrane surface.
Tip: To strengthen cell membranes against potential viral assaults, consider incorporating antioxidants in your diet. These compounds can help bolster membrane integrity by neutralizing oxidative stress, thereby reducing the likelihood of viral entry.
Another critical disruption pathway is the induction of pore formation in the membrane. Certain viruses release proteins that insert themselves into the host membrane, forming channels that destabilize the lipid bilayer. This not only allows viral components to enter the cell but may also lead to cell death. Understanding these mechanisms is crucial for the development of antiviral therapeutics aimed at fortifying membranes or blocking viral entry.
Tip: Regular physical activity can enhance your immune system, supporting your body's ability to respond to viral infections. A robust immune response is essential for maintaining the integrity of biological membranes during an attack.
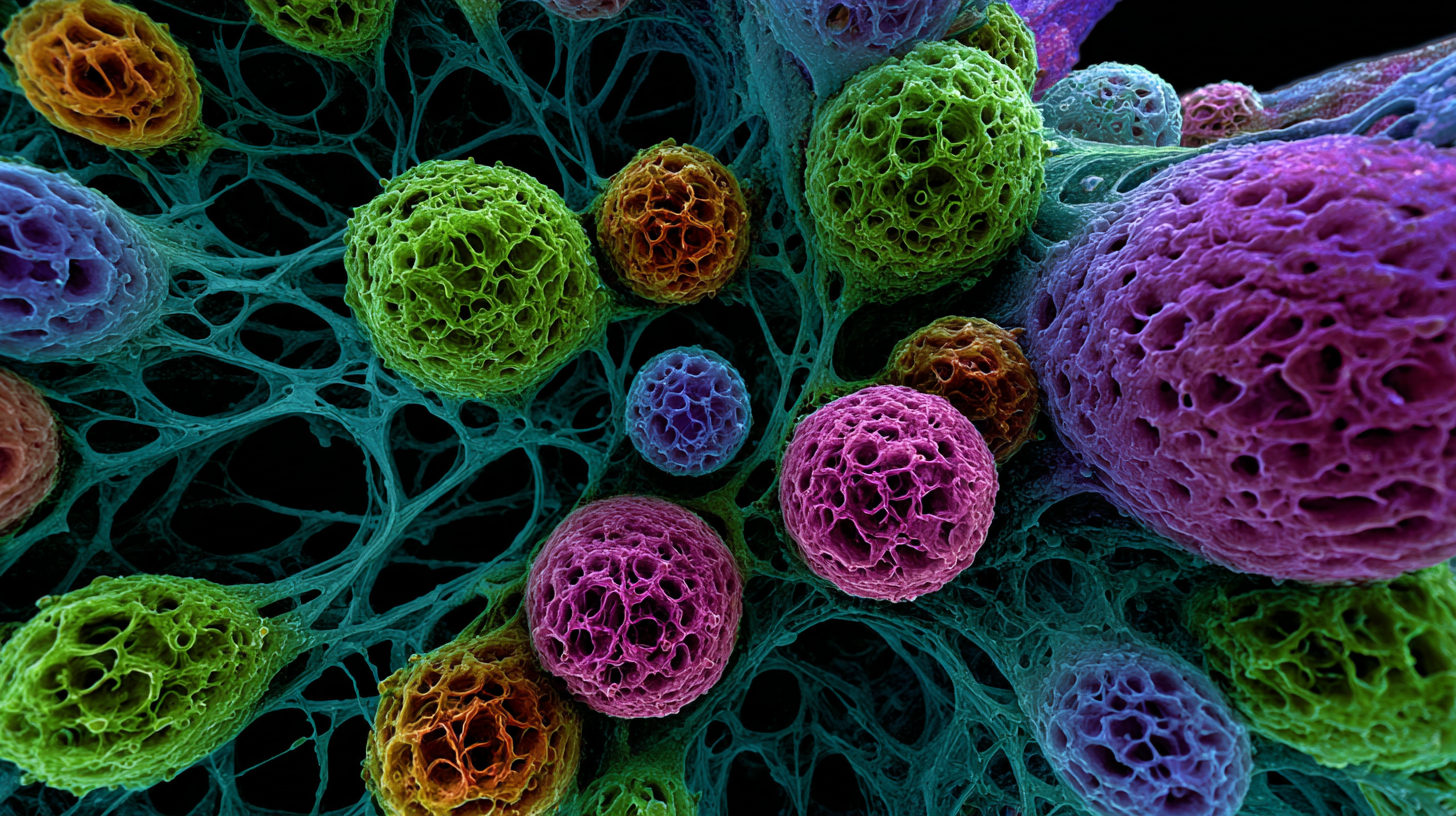
Bacterial biofilm formation on biological membranes is a complex process that poses significant challenges in both clinical and environmental contexts. These biofilms comprise clusters of bacteria that adhere to surfaces, protected by an extracellular matrix that enhances their resistance to antibiotics and the host immune response. Understanding the intricacies of this formation can lead to improved strategies for preventing infections associated with implanted medical devices and water treatment systems.
Tips for tackling biofilm-related issues include regularly monitoring surfaces for early signs of biofilm development. Implementing routine cleaning protocols using biocides can disrupt the biofilm matrix, making it easier to eliminate entrenched bacteria. Additionally, consider utilizing anti-biofilm coatings or materials that minimize bacterial adhesion in high-risk areas. Combining these proactive measures with advanced diagnostic techniques can significantly enhance our ability to manage bacterial infections linked to membrane structures.
Recent studies suggest that the composition of the membrane surface, including its hydrophobicity and charge, plays a crucial role in biofilm formation. By optimizing these surface characteristics, it is possible to inhibit the initial adhesion of bacteria. Furthermore, engaging in further research on the microbial communities within biofilms may provide insights into their behavior and the mechanisms they employ to thrive, ultimately leading to innovative preventive and therapeutic strategies.
The composition of membrane lipids plays a crucial role in determining how cells respond to infections. Biological membranes, primarily composed of phospholipids, cholesterol, and various proteins, serve as protective barriers as well as platforms for signaling. When pathogens invade, the fluidity and asymmetry of the lipid bilayer can significantly influence the susceptibility of cells to infection. For instance, certain lipid species can enhance or inhibit the binding of viral particles, thus meditating the entry of pathogens. The presence of specific lipids, such as sphingolipids, has been linked to increased susceptibility to various viruses, highlighting the intricate relationship between lipid composition and infection mechanisms.
Moreover, the lipid composition of membranes can also impact the immune response. Changes in lipid profiles during inflammation may either bolster or weaken the effectiveness of immune cells in fighting off infections. For instance, high levels of saturated fatty acids can lead to stiffer membranes, potentially impairing the ability of immune cells to migrate to infection sites. On the other hand, unsaturated fatty acids tend to promote membrane fluidity, supporting more effective immune responses. Understanding these lipid-microbe interactions not only sheds light on the fundamental aspects of cellular defenses but also opens potential avenues for therapeutic interventions aimed at modifying membrane compositions to enhance resistance to infections.
Recent advancements in the understanding of biological membrane infection mechanisms have opened new avenues for therapeutic strategies targeting these interactions in infectious diseases. Studies indicate that pathogens often exploit host membrane structures to facilitate entry, evade immune responses, and replicate. For instance, research published in the "Journal of Cell Biology" shows that certain bacteria can manipulate lipid compositions within host membranes, significantly enhancing their infection efficiency. This highlights the critical role that membrane dynamics play in the lifecycle of various pathogens.
Emerging therapeutic strategies derived from these insights focus on disrupting the interactions between pathogens and host membranes. According to a report by the World Health Organization, the global burden of infectious diseases, estimated at over 14 million deaths annually, underscores the urgent need for innovative interventions. Targeting membrane proteins and lipids, as proposed in several clinical trials, has shown promising results in preventing pathogen adhesion and penetration. For example, small-molecule inhibitors designed to interfere with specific lipid-protein interactions have demonstrated a reduction in the virulence of multi-drug resistant strains, offering a ray of hope in the fight against stubborn infectious diseases.






