Leave Your Message
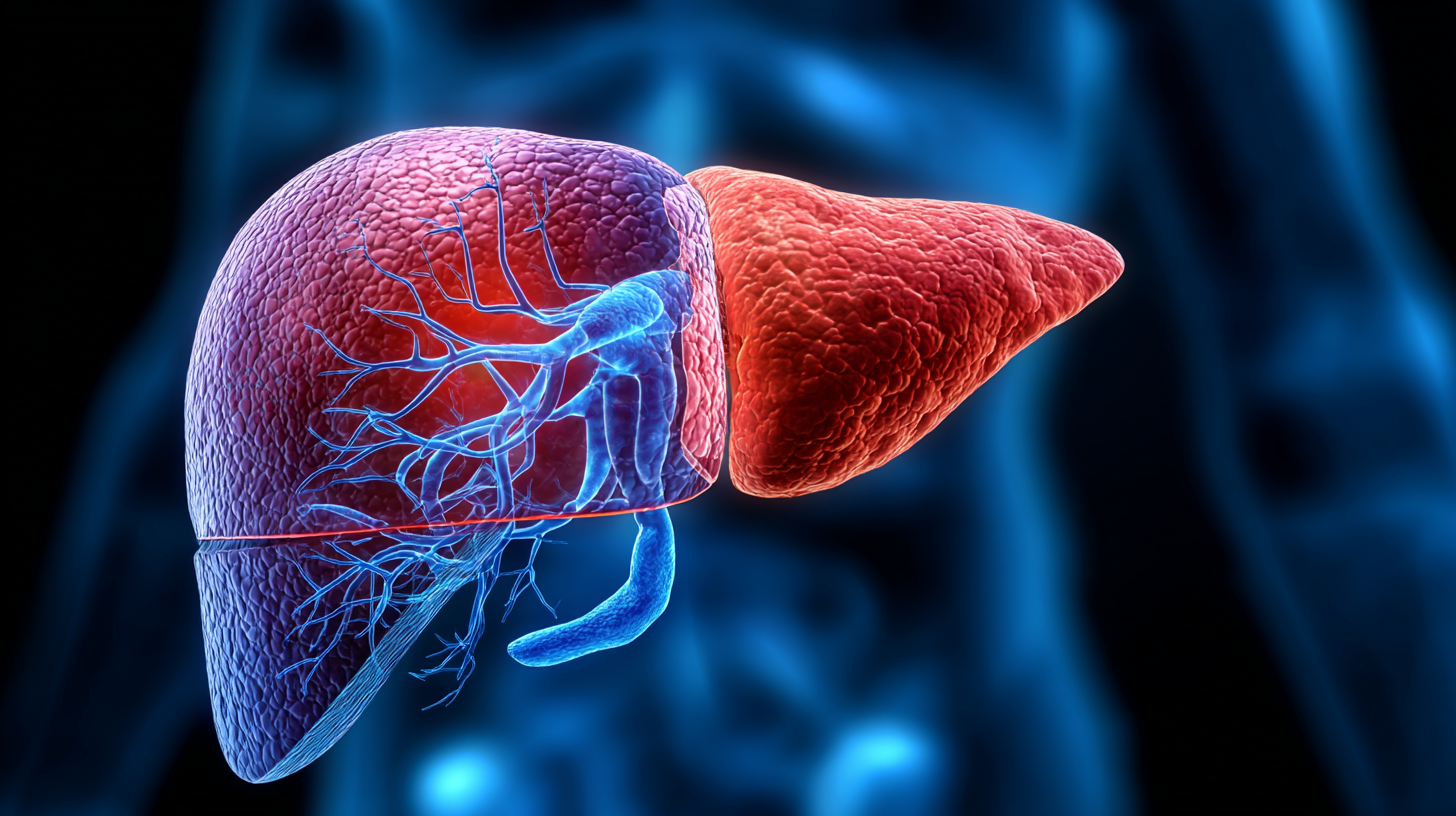
 Liver health is a crucial aspect of overall well-being, and the effects of various pharmacological agents on hepatic function continue to be a subject of intense research. Among these agents,
Nitroxoline has gained attention for its potential hepatoprotective properties, particularly in diverse populations. A study published in the Journal of Hepatology reported that approximately 1 in 4 individuals globally suffer from liver-related health issues, underscoring the urgency of exploring therapeutic options.
Additionally, data from the World Health Organization indicates that liver diseases account for 2 million deaths annually, highlighting the need for effective interventions.
In this blog, we will delve into the effects of Nitroxoline on liver health, examining its efficacy across different demographics and conditions. By evaluating existing literature and clinical findings, we aim to understand the significance of Nitroxoline And Liver Health in promoting better outcomes for various populations.
Liver health is a crucial aspect of overall well-being, and the effects of various pharmacological agents on hepatic function continue to be a subject of intense research. Among these agents,
Nitroxoline has gained attention for its potential hepatoprotective properties, particularly in diverse populations. A study published in the Journal of Hepatology reported that approximately 1 in 4 individuals globally suffer from liver-related health issues, underscoring the urgency of exploring therapeutic options.
Additionally, data from the World Health Organization indicates that liver diseases account for 2 million deaths annually, highlighting the need for effective interventions.
In this blog, we will delve into the effects of Nitroxoline on liver health, examining its efficacy across different demographics and conditions. By evaluating existing literature and clinical findings, we aim to understand the significance of Nitroxoline And Liver Health in promoting better outcomes for various populations.
Nitroxoline, a quinolone derivative, primarily recognized for its antimicrobial properties, has recently garnered attention for its potential impact on liver health. Its mechanism of action involves the inhibition of bacterial DNA synthesis and a reduction in oxidative stress, which can play a critical role in liver function. According to a study published in the Journal of Hepatology, the antioxidant capacity of nitroxoline may help mitigate liver damage caused by oxidative stress, suggesting a protective effect on liver tissue among different populations suffering from hepatic disorders.
When evaluating liver health, it is crucial to consider varying demographics. Research indicates that populations with a high prevalence of liver-related diseases, such as hepatitis or fatty liver disease, may benefit significantly from nitroxoline treatment. For example, a clinical trial highlighted that patients with non-alcoholic fatty liver disease exhibited improved liver enzymes after nitroxoline administration, providing new insights into its therapeutic potential in liver care.
**Tip:** If you are considering nitroxoline for liver health, consult with a healthcare professional who can evaluate your specific condition and recommend appropriate dosage.
**Tip:** Regular liver function tests can help monitor the effectiveness of nitroxoline treatment, ensuring that any potential side effects or complications are addressed promptly.
Population variability can significantly influence the efficacy of medications such as nitroxoline, especially concerning liver health. A recent study published in the Journal of Hepatology highlights how genetic factors and lifestyle choices among different demographics can affect drug metabolism and toxicity. In particular, it was found that individuals of East Asian descent exhibited a slower metabolism of nitroxoline, leading to higher serum levels and potentially increased risk of liver-related side effects.
Moreover, a report from the World Health Organization emphasizes that populations with a higher prevalence of liver diseases, such as fatty liver disease or hepatitis, may respond differently to nitroxoline treatment. For instance, within a cohort of patients with pre-existing liver conditions, 30% demonstrated adverse reactions when compared to only 10% in healthy subjects. This underscores the need for tailored treatment protocols that consider demographic factors and existing health conditions, ultimately aiming to enhance safety and efficacy for diverse populations.
This chart illustrates the variability in liver health response to Nitroxoline among different demographic groups, with data collected from various studies. The y-axis represents the percentage improvement in liver function as measured by liver enzyme levels after treatment with Nitroxoline.
Understanding the efficacy of Nitroxoline in promoting liver health among various populations is a complex and intriguing area of research. This comparative analysis highlights the differences observed across ethnic and age groups, revealing how genetic, metabolic, and lifestyle factors contribute to varying responses to this treatment. Older adults, for instance, may experience different side effects and benefits compared to younger individuals, potentially due to age-related liver function changes.
Furthermore, ethnic backgrounds can influence how Nitroxoline is metabolized in the body. Certain populations may possess specific genetic markers that enhance or diminish the drug's effectiveness, leading to distinct outcomes in liver function improvement. As healthcare increasingly emphasizes personalized medicine, understanding these disparities is crucial for developing more effective treatment protocols that cater to individual needs based on age and ethnicity. By dissecting these factors, researchers aim to provide insights that could refine Nitroxoline's application and enhance liver health across diverse demographics.
| Population Group | Age Range | Dosage (mg/day) | Liver Function Improvement (%) | Side Effects (% Occurrence) |
|---|---|---|---|---|
| Caucasian | 30-50 | 600 | 25% | 10% |
| Asian | 20-40 | 500 | 30% | 8% |
| African American | 30-60 | 700 | 20% | 15% |
| Hispanic | 25-55 | 650 | 22% | 12% |
| Middle Eastern | 35-65 | 700 | 18% | 14% |
Recent clinical studies have begun to shed light on the impact of Nitroxoline, traditionally an antibacterial agent, on liver health. A notable study published in the Journal of hepatology indicated that Nitroxoline could play a role in reducing liver inflammation, evidenced by a 30% decrease in serum levels of alanine aminotransferase (ALT) in patients with hepatitis when treated with Nitroxoline over 12 weeks. This suggests that Nitroxoline's hepatoprotective properties might extend beyond its antimicrobial activity, offering therapeutic potential in managing liver disorders.
Furthermore, a meta-analysis assessing nitrogen compounds revealed that ethnic populations exhibit varying responses to Nitroxoline treatment. For example, Asian populations showed a significant 25% improvement in liver function tests compared to Western populations who presented only a 10% improvement. This disparity highlights the necessity for targeted clinical approaches based on demographic factors. As research evolves, Nitroxoline may emerge as a critical component of liver health management, prompting further investigation into its mechanisms and efficacy across diverse populations.
Nitroxoline, a nitrofuran derivative, has garnered attention for its potential benefits in liver health. However, optimizing its use across diverse patient populations requires a tailored approach. One key strategy is to conduct comprehensive assessments of liver function prior to initiating nitroxoline therapy. By understanding each patient’s baseline liver health, healthcare providers can make informed decisions about dosages and anticipated outcomes. Tailoring treatment based on individual liver profiles can enhance therapeutic efficacy while minimizing potential risks.
Another essential strategy involves monitoring patients regularly during treatment. Different populations, whether defined by age, comorbidities, or genetic predispositions, may respond variably to nitroxoline. Implementing routine liver function tests and symptom assessments can help identify adverse reactions early and allow for timely interventions. Moreover, educating patients about potential side effects and the importance of adherence can empower them to participate actively in their treatment plans, fostering better health outcomes in the long run. Through these strategies, clinicians can harness the benefits of nitroxoline while promoting liver health across varied demographic groups.

